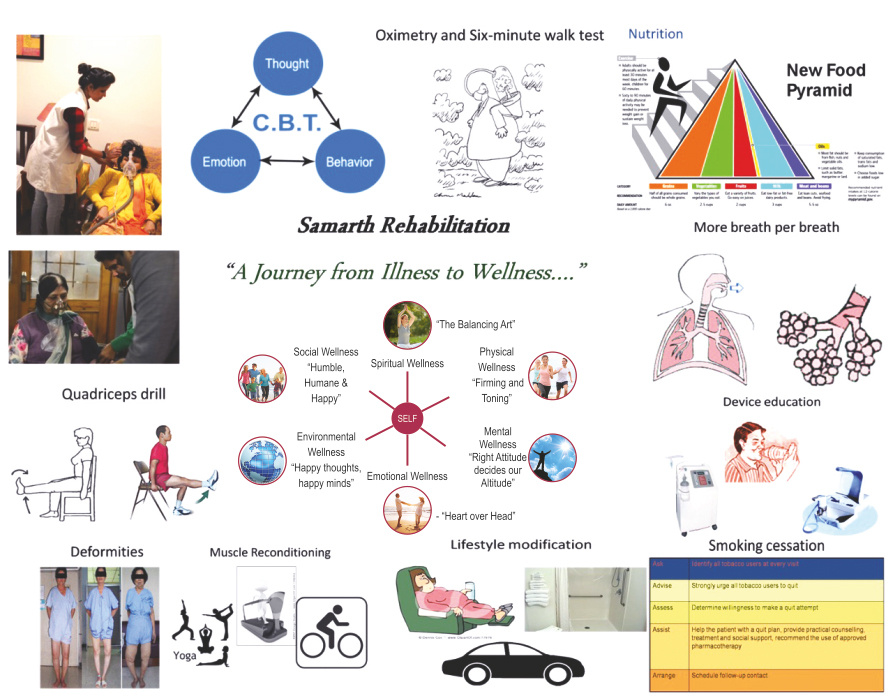
" A Journey from Illness to Wellness"
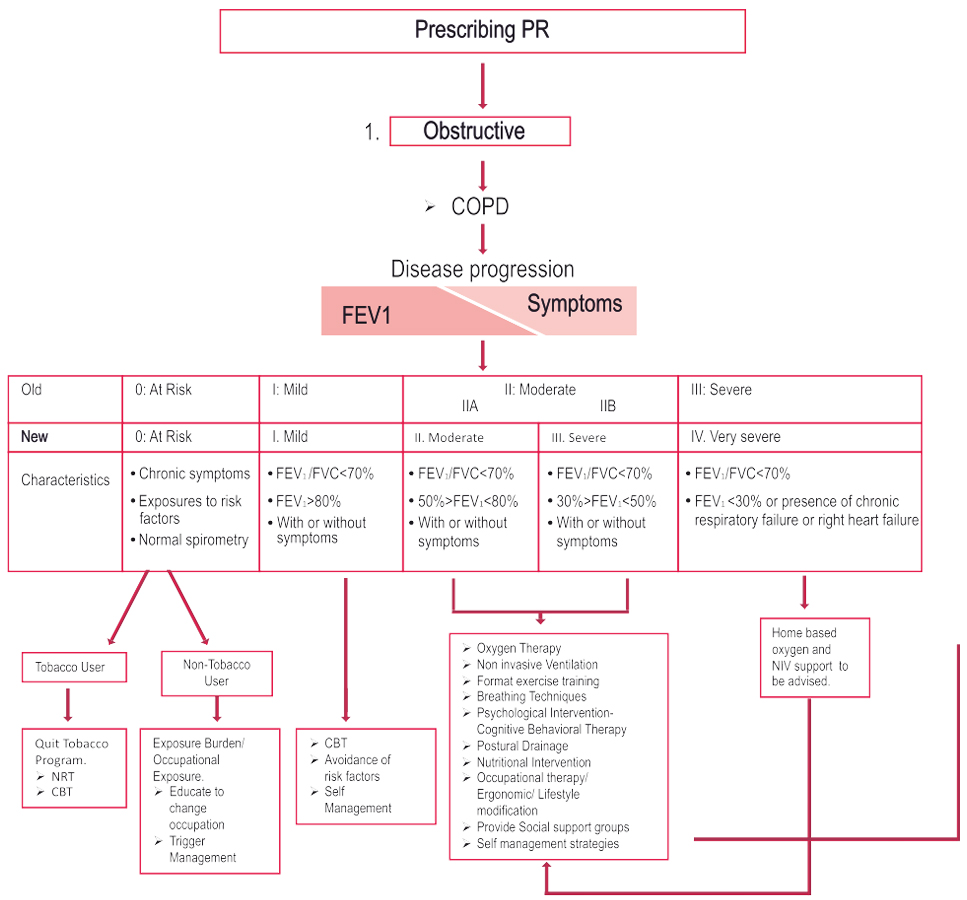
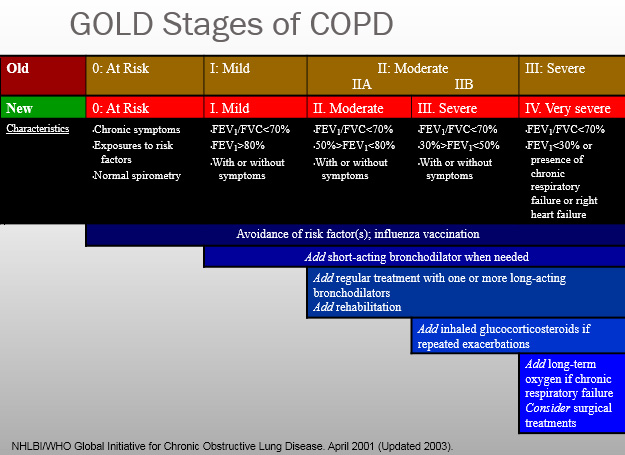
Pulmonary Rehab Algorithm
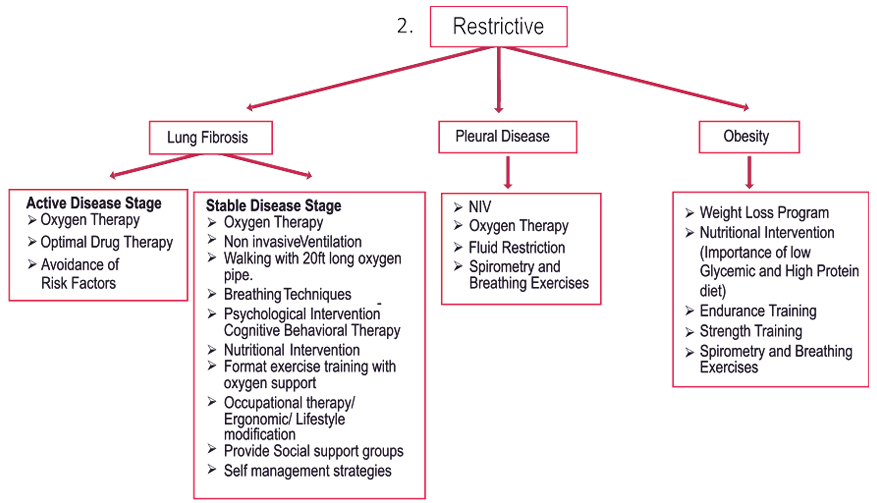
Key Points

Components of a Comprehensive Program
> Assessment
> Education
> Exercise Training
> Psychosocial/Behavioral intervention
> Nutrition
> Breathing techniques
> Medications, devices & specific therapy
> Outcome Assessment
Rehabilitation tries to address morbidities and their consequences through education and exercise. Patients are encouraged to become more actively involved in their own health care, more independent in ADLs and less dependent on health professionals and expensive medical resources. Rather than focusing solely on reversing disease processes, rehab attempts to reduce symptoms and make individual more functional
Purpose
Restore function following an illness or injury, with the goal of maximizing a person’s ability to achieve fullest life possible
Who can benefit?
- Chronic respiratory disease symptomatic with optimum drug therapy
- Chronic cardiovascular diseases with breathlessness despite optimum intervention and drug therapy
- Chronic neurological diseases
- Chronic orthopaedic diseases& post operative
- Lifestyle disoders like Stress,Sleep , Obesity
- Special children
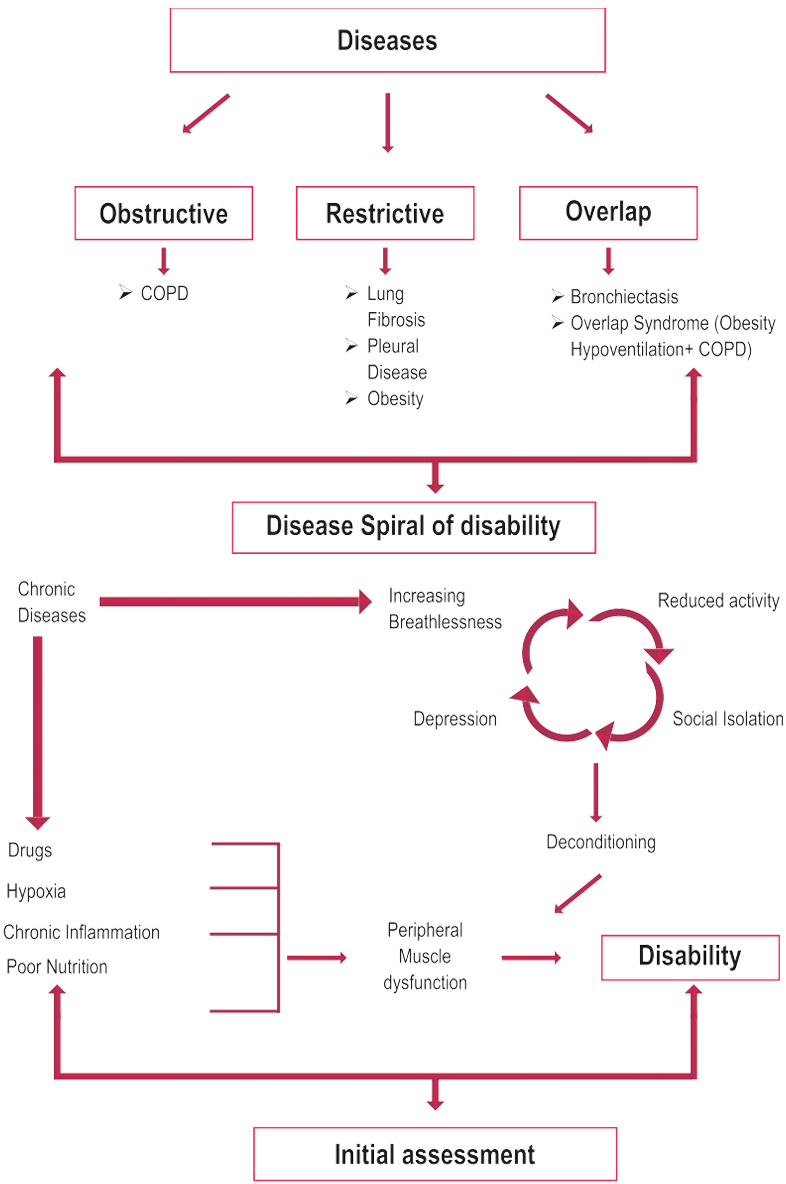
Consequences of advanced chronic diseases
- Peripheral Muscle dysfunction
- Respiratory muscle dysfunction
- Nutritional abnormalities
- Cardiac impairment
- Skeletal disease
- Sensory defects
- Neuro cognitive dysfunction
- Psychosocial dysfunction
Mechanisms for these morbidities
- Deconditioning
- Malnutrition
- Effects of hypoxemia
- Steroid myopathy
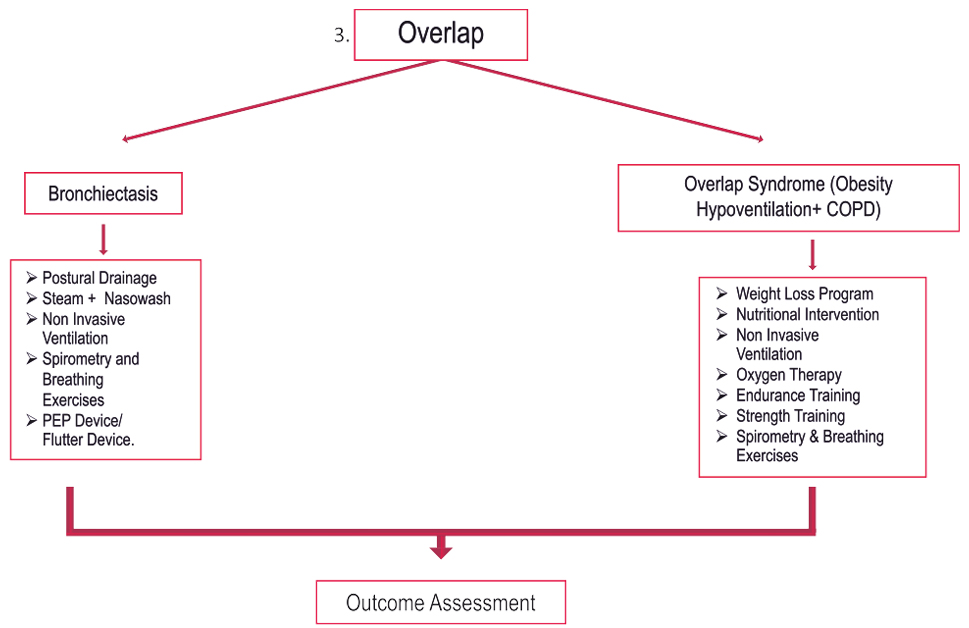
- Hyperinflation
- Diaphragmatic fatigue
- Psychosocial dysfunction from anxiety, guilt, dependency and sleep disturbances.
Benefits
- Improved Exercise Capacity
- Reduced perceived intensity of dyspnea
- Improve health-related QOL
- Reduced hospitalization
- Reduced anxiety and depression
- Improved limb function
- Benefits extend well beyond immediate period of training.
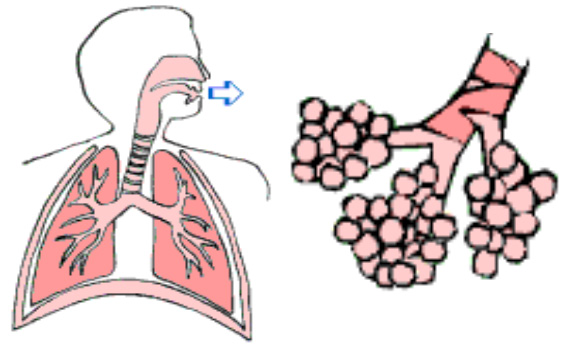
Causes of Dyspnea in COPD
narrowed airways (bronchospasm, increased compliance airway secretions, airway thickening, increased cholinergic tone)
Consequences of advanced COPD
- Peripheral Muscle dysfunction
- Respiratory muscle dysfunction
- Nutritional abnormalities
- Cardiac impairment
- Skeletal disease
- Sensory defects
- Psychosocial dysfunction
Mechanisms for these morbidities
- Deconditioning
- Malnutrition
- Effects of hypoxemia
- Steroid myopathy or ICU neuropathy
- Hyperinflation
- Diaphragmatic fatigue
- Psychosocial dysfunction from anxiety, guilt, dependency and sleep disturbances.
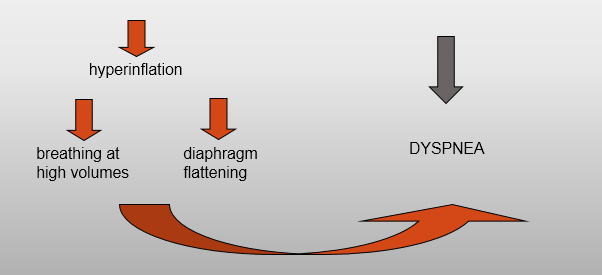
Pulmonary Rehabilitation
“A multidisciplinary continuum of services directed to persons with pulmonary diseases and their families, usually by an interdisciplinary team of specialists, with the goal of achieving and maintaining the individual’s maximum level of independence and functioning in the community”
Benefits of Pulmonary Rehab.
The benefits are seen in irreversible pulmonary disorders because much of the disability is not from the lung disease but from the secondary morbidities.
Objective Abnormalities
- FEV1 less than 80% predicted
- FEV1/FVC less than 70 %
- DLCO less than or equal to 65% of predicted
- Resting hypoxemia less than or equal to 90%
- Exercise Testing demonstrating hypoxemia less than 90%
- Enrolling active smokers is controversial but they may benefit significantly with a focus on smoking cessation.
- Patient Motivation is a necessary consideration.
Setting for Pulmonary Rehabilitation
- Outpatient
- Inpatient
- Home
- Community Based
- Choice varies depending on
- Distance to program
- Insurance payer coverage
- Patient preference
- Physical, functional, psychosocial status of patient
Components of a Comprehensive Program
- Exercise Training
- Education
- Medication and other therapies
- Psychosocial/behavioral intervention
- Chest – physical therapy
- Nutrition assessment
- Outcome Assessment
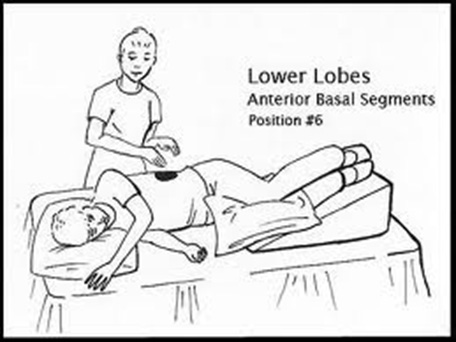
Chest Physical Therapy
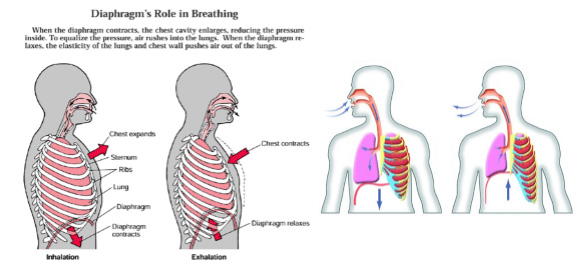
- Pursed Lip Breathing – shifts breathing pattern and inhibits dynamic airway collapse.
- Posture techniques – forward leaning reduces respiratory effort, elevating depressed diaphragm by shifting abdominal contents.
- Diaphragm Breathing – Some patients with extreme air trapping and hyperinflation have increased WOB with this technique
- Postural Draining – valuable in patients who produce more than 30cc/24 hours/ Coughing techniques
Nutritional Assessment
- Diet history, BMI
- Over or Under weight.
- Classes in weight management and/or nutritional counseling to improve weight management
Outcome Assessment
- An important component of pulmonary rehabilitation, being used to determine individual patient responses and evaluate overall effectiveness of program.
- Dyspnea 10 pt scale, Borg scale, Visual Analog Scale
- Exercise Ability – Borg Scale, 6MDW/Progressive exercise testing pre and post rehab.
- Health Status – Respiratory-related QOL; CRDQ
- Activity Levels –Respiratory-Specific functional Status, Duke Functional Status Scale.
Quit Smoking

Motivation

More breath per breath
Pursed lip breathing

Diaphragmatic breathing
Mucus clearing and postural drainage
Device education

Oximetry and Six-minute walk test
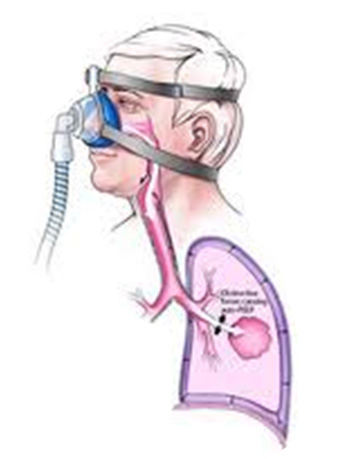
Non-invasive ventilation